In healthcare's ever-evolving and life-saving landscape,
Patient Blood Management (PBM) is a pivotal approach to reshaping how patients and medical professionals view and handle blood use in clinical settings. This article delves into the concept of PBM, highlighting its significance and the many benefits Patient Blood Management offers patients and doctors.
What is Patient Blood Management?
We'll start with the most critical question for those who don't know the term: what exactly is PBM?
Patient Blood Management is a patient-centred, systematic, evidence-based approach to improving patient outcomes. It focuses on managing and preserving a patient's blood while promoting patient safety and empowerment. This approach is applied across three main pillars:
• Optimising erythropoiesis (including red cell mass and iron stores),
• Minimising blood loss and bleeding, and
• Harnessing and optimising the patient-specific physiological reserve of anaemia while treatment is initiated.
These pillars are implemented in three phases: pre-operative, intra-operative, and post-operative (before, during, and following specific treatment). Patient blood management aims to effectively manage the patient's blood and haemopoietic system, like how other organs and organ systems are managed during patient care. This approach ensures that blood's unique and vital human resource is appropriately managed and maintained in health and disease. In addition, PBM emphasises the conservation of a patient's blood and minimising or avoiding the need to transfuse allogeneic blood components.

PBM - Benefits for Patients
Patient Blood Management offers significant benefits directly to patients.
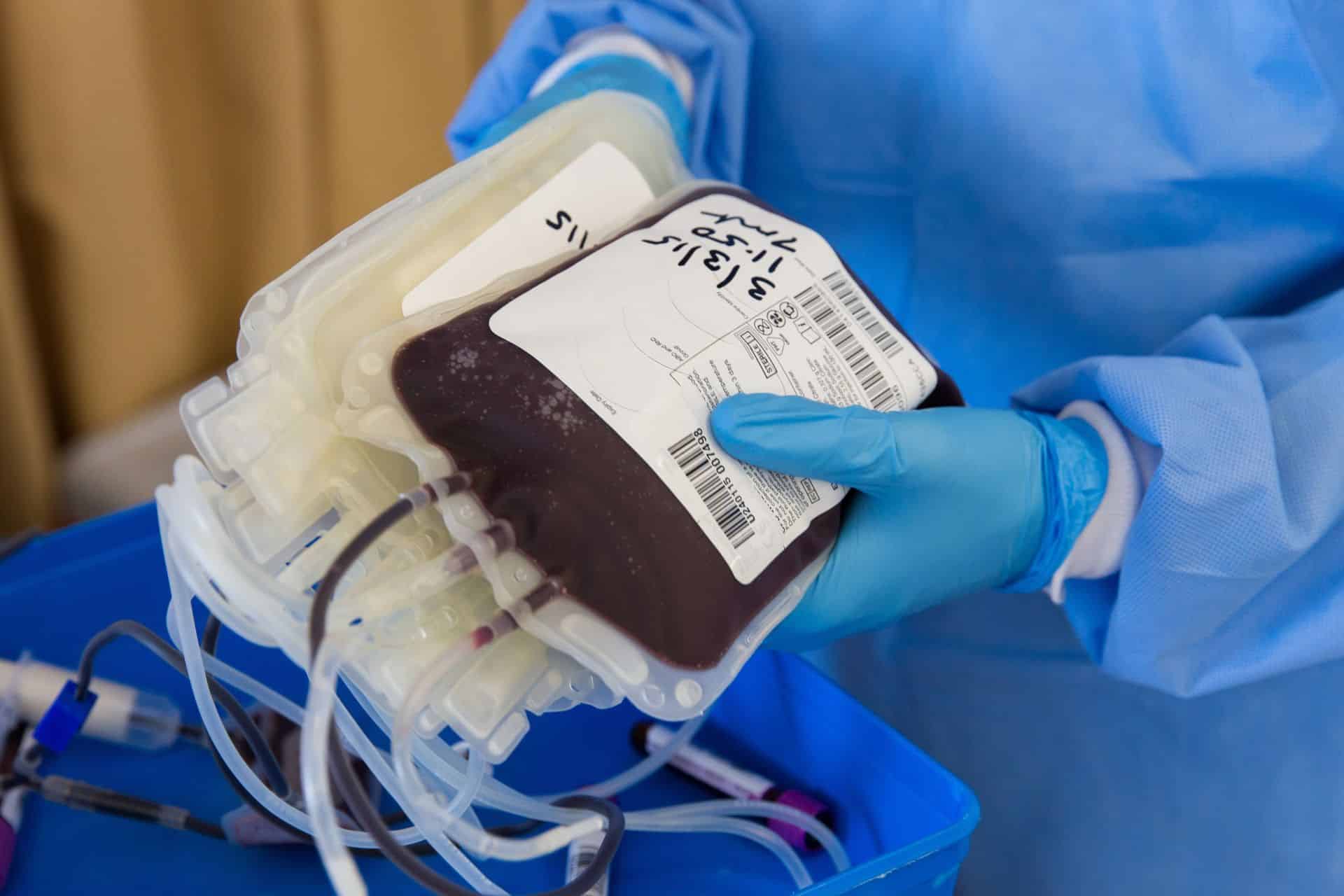
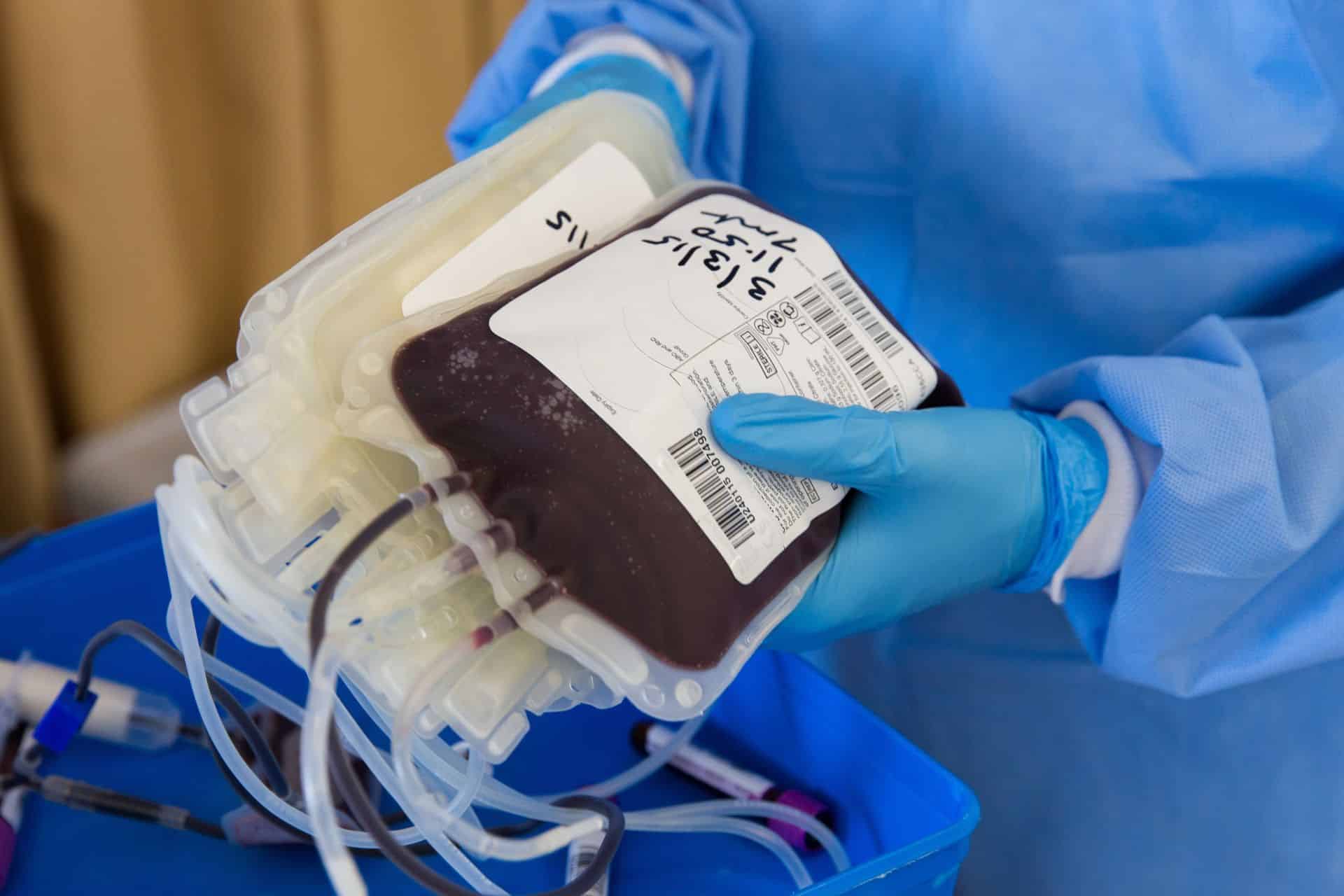
One of the primary advantages of PBM is the reduced risk of complications related to blood transfusions. While sometimes necessary, blood transfusions can carry risks like allergic reactions, infections, and immune system responses. Some in the medical community, like Dr. Denton Cooley, have long believed that replacing blood can have the same effect as replacing any organ; the body can reject the replacement. By minimising or even avoiding transfusions, Patient Blood Management helps lower these risks, leading to safer patient treatment processes.
Yes, a critical benefit is the improvement in patient outcomes. PBM strategies involve optimising a patient's health before any surgical or medical intervention, focusing on their own blood management. This approach has been linked to better outcomes, shorter hospital stays, and, in some cases, lower mortality rates. These improved outcomes are a direct result of the proactive management of a patient's blood health.
Additionally, Patient Blood Management can lead to enhanced recovery for patients. Since the approach emphasises the patient's overall health and optimal management of their blood, it often results in a quicker and more comfortable recovery process.
PBM is patient-centered, tailoring medical care to each patient's individual needs and conditions. This personalised approach ensures that each patient receives the most appropriate and effective treatment, which is crucial for their health and well-being.

PBM - Advantages for Healthcare Professionals
But is Patient Blood Management only suitable for patients? No, PBM also offers several benefits for health professionals, impacting how they deliver care and manage resources.
One key benefit is the enhancement of clinical decision-making. How? Well, PBM provides a framework for health professionals to make informed, evidence-based decisions regarding patient care, particularly in managing blood resources. The PBM framework encourages a more holistic view of patient care, where blood management is integrated into the broader context of the patient's overall health and treatment plan.
Patient Blood Management brings together various healthcare professionals, such as surgeons, anesthesiologists, haematologists, and nurses, fostering collaboration and communication. This teamwork is essential for comprehensive patient care and helps develop more coordinated and effective treatment strategies.
There's also an educational aspect to Patient Blood Management; it encourages continuous learning and adaptation of new research findings and techniques among health professionals. This ongoing education ensures that healthcare providers stay current with the best practices in blood management, ultimately improving the quality of care provided.
Following Patient Blood Management guidelines can lead to a more efficient use of healthcare resources. By reducing the reliance on blood transfusions, it helps in conserving blood supplies, which are often limited. This efficient use of resources is beneficial in terms of cost and ensuring that blood products are available for those who need them the most.
Lastly, Patient Blood Management aligns with the healthcare industry's growing emphasis on patient-centered care. By adopting PBM protocols, health professionals are better equipped to provide care that prioritises the patient's needs and conditions, which is increasingly recognised as an essential component of high-quality healthcare.
In essence, PBM provides health professionals with a structured approach to blood management, enhancing clinical decision-making, promoting interdisciplinary collaboration, encouraging continuous learning, ensuring efficient resource utilisation, and aligning with patient-centred care principles.

Patient Blood Management in Action
Patient Blood Management has been effectively implemented in various clinical settings, demonstrating its value in improving patient outcomes, particularly in surgical environments. Here are some highlights of the effectiveness of PBM in action:
Reduction in Transfusion Needs: According to the article Patient Blood Management: Effectiveness and Future Potential published in the journal Anesthesiology July 2020 (Vol. 133, 212–222), Patient Blood Management strategies have significantly reduced the need for blood transfusions in surgical patients. This is a crucial outcome, as reducing transfusions minimises the risks associated with transfusion-related complications. For instance, studies have shown that treating preoperative anaemia in orthopaedic surgery with intravenous iron and subcutaneous erythropoietin decreased erythrocyte transfusion rate, nosocomial infections, and hospital stays.
Large-Scale Effectiveness: A significant study involving over 1.2 million patients analysed the impact of Patient Blood Management in a hospital setting. This study found a substantial reduction in the utilisation of red blood cells for transfusions after implementing PBM. Specifically, the study observed a relative decrease of 13.9% in the number of red blood cell units transfused per 1000 patients. Additionally, the overall safety of PBM was validated as the rate of in-hospital mortality and postoperative complications was comparable before and after PBM implementation, demonstrating its non-inferiority in terms of patient safety.
These findings collectively illustrate that Patient Blood Management effectively reduces the need for and risks associated with blood transfusions, maintains patient safety, and improves overall surgical outcomes. Implementing PBM protocols in diverse healthcare settings and surgical disciplines further underscores its broad applicability and effectiveness in modern medical practice.
Final Thoughts on Patient Blood Management
As explored throughout this article, Patient Blood Management emerges as a medical approach and a revolutionary paradigm in healthcare. It interlinks the intricate complexities of medical science with the humane touch of patient-centred care, creating a tapestry of improved outcomes, safer practices, and more efficient healthcare delivery.
At its core, Patient Blood Management goes above traditional blood management methods, redefining how medical practitioners approach blood conservation and patient care. By optimising each patient's blood health and reducing the reliance on transfusions, Patient Blood Management aligns with the ethical imperative of doing no harm – a cornerstone of medical practice. This approach safeguards the patient against potential transfusion-related risks and opens doors to swifter recoveries and enhanced overall well-being.
Moreover, the effects of Patient Blood Management extend beyond the individual patient. It ushers in a new era of resource efficiency, benefiting the healthcare system. The conservation of blood supplies, a crucial yet often limited resource, and the reduction in healthcare costs underscore PBM's role as a medical and economic efficiency steward.
The evidence backing Patient Blood Management effectiveness, from large-scale studies to individual case reports, paints a vivid picture of its impact. This body of evidence validates PBM's role in current medical practice and underscores its potential as a standard across healthcare systems globally.
In essence, Patient Blood Management is more than a clinical protocol; it is a testament to the evolving nature of healthcare, where patient welfare and resource optimisation combine. As we look to the future, Patient Blood Management is setting the standard, guiding the way towards a more holistic, patient-centric, and sustainable healthcare practice. This approach is poised to reshape the healthcare landscape, ensuring that patient safety, quality care, and resource efficiency remain at the forefront of medical endeavours.
Want More Information on PBM?
There are many sources you can turn to if you want to learn more about PBM. However, the most authoritative source would have to be patientbloodmanagement.org and their
Patient Blood Management resource library. They have a large library of resources for medical professionals and information for patients alike!
Appendix: Medical Terminology
Erythropoiesis: The process of creating and controlling quantities of red blood cells.
Red cell mass and iron stores: Components related to the quantity and quality of red blood cells and the body's iron reserves.
Anaemia: A condition where the number or quality of red blood cells is deficient.
Haemopoietic system: The body system responsible for producing blood cells.
Allogeneic blood components: Blood products are donated from one person to another.
Transfusion-related complications: Adverse reactions or issues arising from receiving a blood transfusion.
Nosocomial infections: Infections acquired in a hospital setting.
Intravenous iron and subcutaneous erythropoietin: Medical treatments used to manage anaemia and related conditions.
Erythrocyte transfusion rate: The frequency or rate at which red blood cell transfusions are administered.
Non-inferiority: A term used in clinical trials indicating that a new treatment is not worse than an existing treatment.